Understanding how past wounds can become pathways to deeper connection
Marriage vows promise “for better or worse,” but few couples anticipate how past trauma can profoundly shape their relationship. When one partner carries invisible wounds from their history, it affects everything from daily conversations to intimate moments. Yet with understanding and intentional care, these challenges can become opportunities for unprecedented closeness and resilience.
When the Past Lives in the Present
Sarah freezes when her husband Mark raises his voice—even during playful moments. What Mark doesn’t initially understand is that his tone triggers memories of an unpredictable childhood, making Sarah’s nervous system react as if danger is imminent.
Similarly, Emily physically healed from a serious car accident, but her body remembers the trauma. Highway driving now feels impossible, creating tension whenever she and her husband, David, plan trips together.
These scenarios illustrate what trauma expert Dr. Bessel van der Kolk describes in The Body Keeps the Score: trauma literally reshapes how our brains and bodies perceive safety and connection. For partners, understanding this isn’t just helpful—it’s transformative.
The Ripple Effects: How Trauma Touches Every Corner of Marriage
Emotional Landscapes
Living with trauma often means experiencing intense emotional swings—from overwhelming anxiety to profound numbness. Your partner might seem to “shut down” or react strongly to seemingly small triggers, leaving you feeling like you’re walking on eggshells.
Communication Barriers
Trauma can make it incredibly difficult to articulate internal experiences. What feels like defensiveness or withdrawal might actually be your partner’s nervous system protecting them from perceived threats.
Intimacy Challenges
Both emotional and physical closeness can feel threatening when trauma has shattered someone’s sense of safety. Touch, vulnerability, and even eye contact might trigger distressing memories or sensations.
Trust and Connection
Even in loving relationships, trauma can create persistent doubts about safety, consistency, and loyalty. This isn’t about you personally—it’s about how trauma rewires the brain’s threat-detection systems.
Daily Life Disruptions
Chronic anxiety, sleep disturbances, concentration difficulties, and avoidance behaviors can affect everything from household routines to social activities.
The Hidden Impact on Supporting Partners
While focus naturally centers on the trauma survivor, supporting partners face their own challenges that deserve recognition and care.
Secondary trauma can develop from repeatedly witnessing your partner’s pain or hearing traumatic details. You might experience:
- Emotional exhaustion and anxiety
- Sleep disruption and irritability
- Feelings of helplessness or inadequacy
- Isolation from the unique nature of your situation
Relationship dynamics can shift dramatically:
- Feeling more like a caregiver than an equal partner
- Frustration when your support efforts seem ineffective
- Resentment about lost spontaneity or social activities
- Guilt about having your own needs and feelings
Remember: Acknowledging these impacts isn’t selfish—it’s essential for sustaining your ability to support your partner and maintain your own well-being.
Building Your Trauma-Informed Partnership: A Roadmap
1. Invest in Individual Therapy
This is your foundation. Both partners benefit from professional support:
- For trauma survivors: Processing experiences safely and developing coping tools
- For supporting partners: Managing secondary trauma and maintaining emotional health
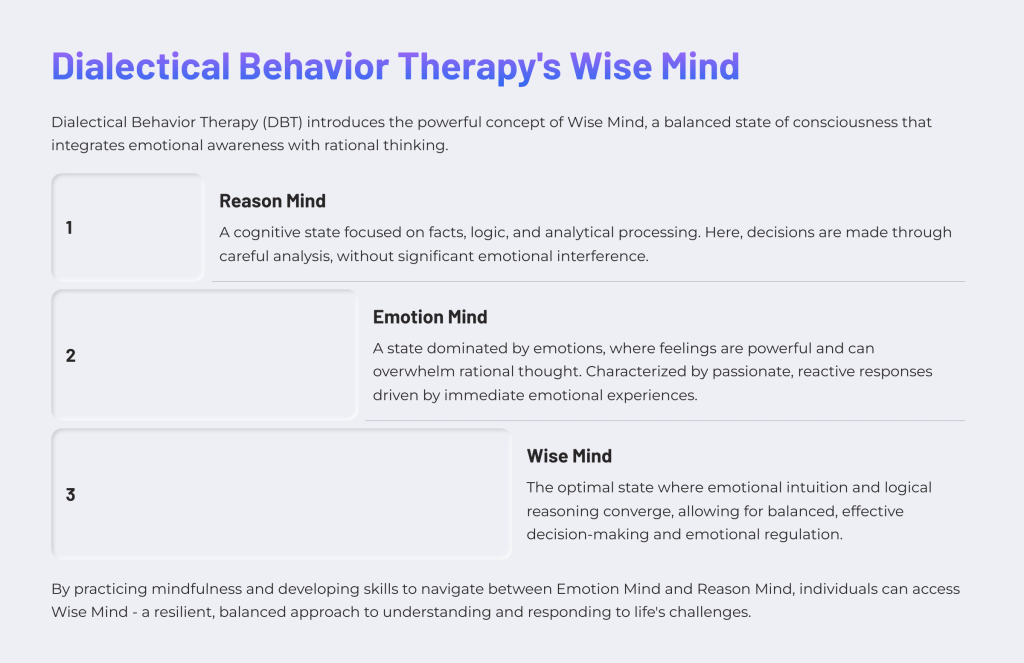
2. Become Trauma-Literate Together
Understanding how trauma affects the nervous system transforms confusion into compassion. When you recognize that your partner’s “overreactions” are actually their brain protecting them from perceived danger, everything changes.
Key insight: Those fight, flight, freeze, or fawn responses aren’t choices—they’re automatic survival mechanisms.
3. Practice Compassionate Communication
- Lead with curiosity instead of judgment
- Recognize when someone is triggered and focus on safety first
- Use “I” statements to express your own needs
- Create agreements about how to handle overwhelming moments
4. Embrace the Marathon Mindset
Trauma healing isn’t linear. There will be breakthroughs followed by setbacks, as well as good weeks and difficult ones. Progress might look like three steps forward, two steps back—and that’s completely normal.
5. Co-Create Safety
Transform your relationship into a haven by:
- Establishing predictable routines when possible
- Learning nervous system regulation techniques together (breathing exercises, grounding techniques, mindful movement)
- Identifying and minimizing environmental triggers
- Developing safety signals and check-in practices
6. Consider Trauma-Informed Couples Therapy
A therapist specializing in trauma can guide you through rebuilding trust, improving communication, and navigating intimacy challenges. Generally, this approach works best after the trauma survivor has established some degree of individual stability.
7. Prioritize Your Own Oxygen Mask
For supporting partners, self-care isn’t optional—it’s essential for everyone’s wellbeing:
- Maintain friendships and hobbies outside the relationship
- Set healthy boundaries around what you can and cannot do
- Seek your own support through therapy, support groups, or trusted friends
- Remember that you can’t heal your partner’s trauma for them
The Unexpected Gift
While navigating trauma’s impact on marriage presents real challenges, many couples discover something remarkable: trauma can become a pathway to extraordinary intimacy and resilience. When you learn to hold space for each other’s deepest vulnerabilities, when you develop skills to co-regulate during difficult moments, when you choose understanding over judgment, you create a bond that can weather almost anything.
The marriage that emerges from this crucible often becomes stronger, more authentic, and more compassionate than many couples ever experience. It’s a relationship that truly embodies “for better or worse”—not because it’s easy, but because it’s real.
If you’re navigating trauma in your relationship, remember that seeking help is a sign of strength, not weakness. Consider reaching out to a trauma-informed therapist who can provide personalized guidance for your unique situation.
Resources:
- “The Body Keeps the Score” by Bessel van der Kolk
- Psychology Today’s therapist directory (filter for trauma specialists)
- National Center for PTSD resources for families
- Local support groups for trauma survivors and their partners