Finding A Pathway to Healing
Traumatic memories can cast long shadows over our lives, affecting our mental, emotional, and physical well-being. Whether stemming from childhood abuse, accidents, or other life-altering events, these memories can remain buried in our subconscious, influencing our behavior and thoughts in ways we may not fully understand. Though often challenging and painful, confronting these memories is crucial to healing and reclaiming control over our lives.
The Nature of Traumatic Memories
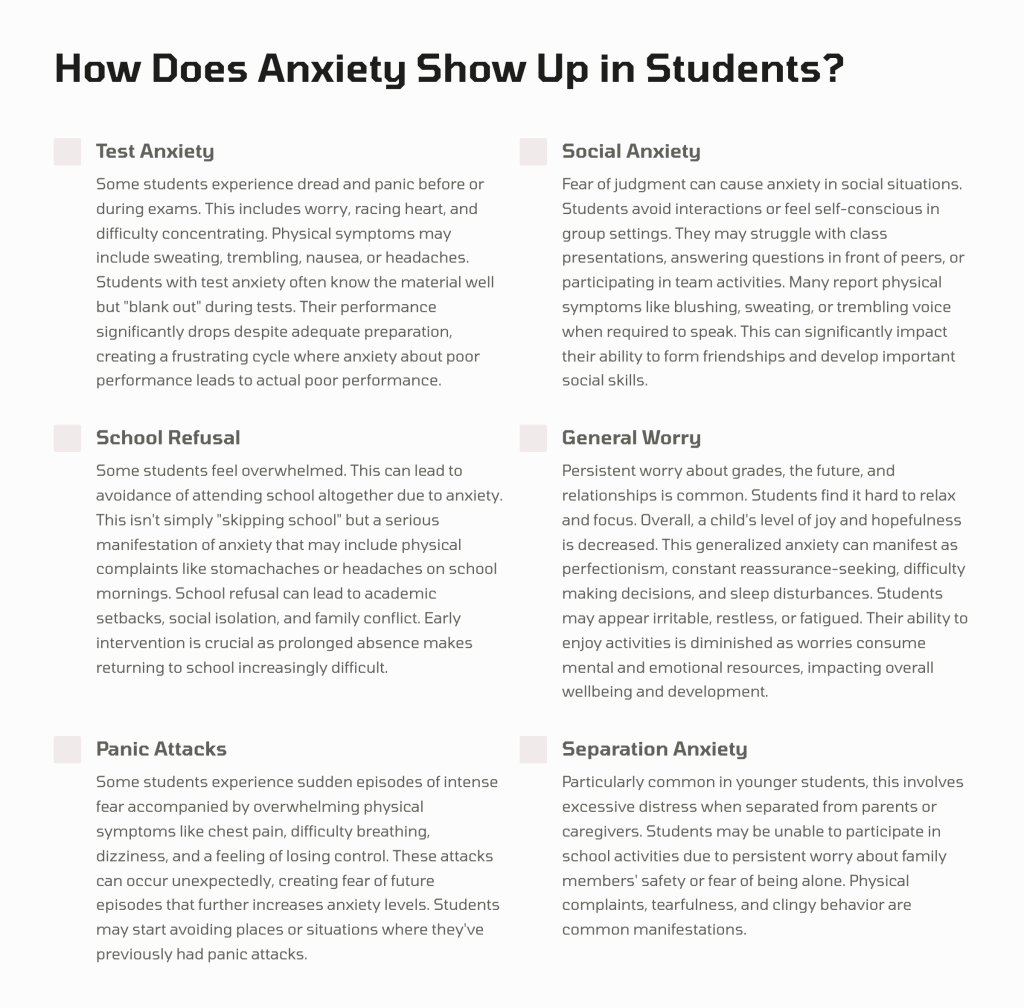
Traumatic memories differ from regular memories in intensity and how they are stored in the brain. They often remain fragmented and disjointed, resurfacing unexpectedly and triggering intense emotional and physical reactions. These memories can lead to symptoms of PTSD, anxiety, depression, and other mental health issues if not addressed.
Why Confront Traumatic Memories?
1. Breaking the Cycle of Avoidance
Avoidance is a common coping mechanism for dealing with trauma. We may avoid places, people, or situations that remind us of the traumatic event. While this can provide temporary relief, it often reinforces the trauma, making it more challenging to manage in the long run. Confronting traumatic memories helps break this cycle, reducing the power they hold over us.
2. Processing and Integration
Facing traumatic memories allows for the processing and integrating these experiences into our broader life narrative. This process can transform fragmented, distressing memories into coherent stories we can understand and accept. This integration diminishes the emotional charge associated with these memories, reducing their impact on our daily lives.
3. Regaining Control
Trauma can leave us feeling powerless and out of control. By confronting our traumatic memories, we reclaim agency over our experiences. This empowerment is a critical step in healing, allowing us to move from being victims of our past to active participants in our recovery.
4. Improving Mental and Physical Health
Unresolved trauma is linked to a range of mental and physical health issues, including chronic stress, anxiety, depression, and even physical ailments like cardiovascular disease and weakened immune function. Addressing traumatic memories can alleviate these symptoms, improving overall health and well-being.
How to Confront Traumatic Memories Safely
1. Seek Professional Support
Working with a mental health professional trained in trauma-informed care is essential. Therapies such as Cognitive Behavioral Therapy (CBT), Eye Movement Desensitization and Reprocessing (EMDR), and Somatic Experiencing can provide structured and supportive environments to process traumatic memories.
2. Create a Safe Environment
Ensure that you are in a safe, supportive environment when addressing traumatic memories. This might involve creating a comfortable physical space, having trusted friends or family members nearby, and practicing self-care routines promoting safety and stability.
3. Take it Slow
Confronting trauma is not a race. It’s essential to go at your own pace and not force yourself to relive painful experiences before you’re ready. Gradual exposure and processing are key to ensuring the process is therapeutic rather than re-traumatizing.
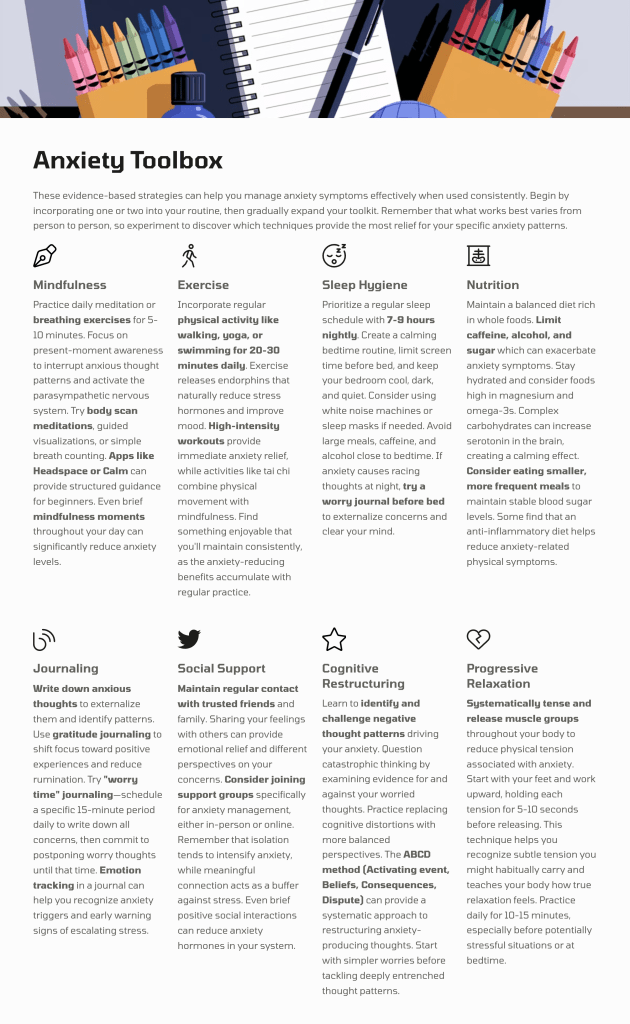
4. Use Grounding Techniques
Grounding techniques can help manage intense emotions and connect you to the present moment. Techniques such as deep breathing, mindfulness, and focusing on physical sensations can provide immediate relief when confronting difficult memories.
Confronting traumatic memories is a challenging but vital step towards healing. By facing these memories, we can break the cycle of avoidance, process and integrate our experiences, regain control, and improve our overall health. With the support of trained professionals and a safe, gradual approach, we can transform our trauma from a source of pain into a pathway to resilience and growth. Remember, the healing journey is personal and unique—take it one step at a time and honor your progress.
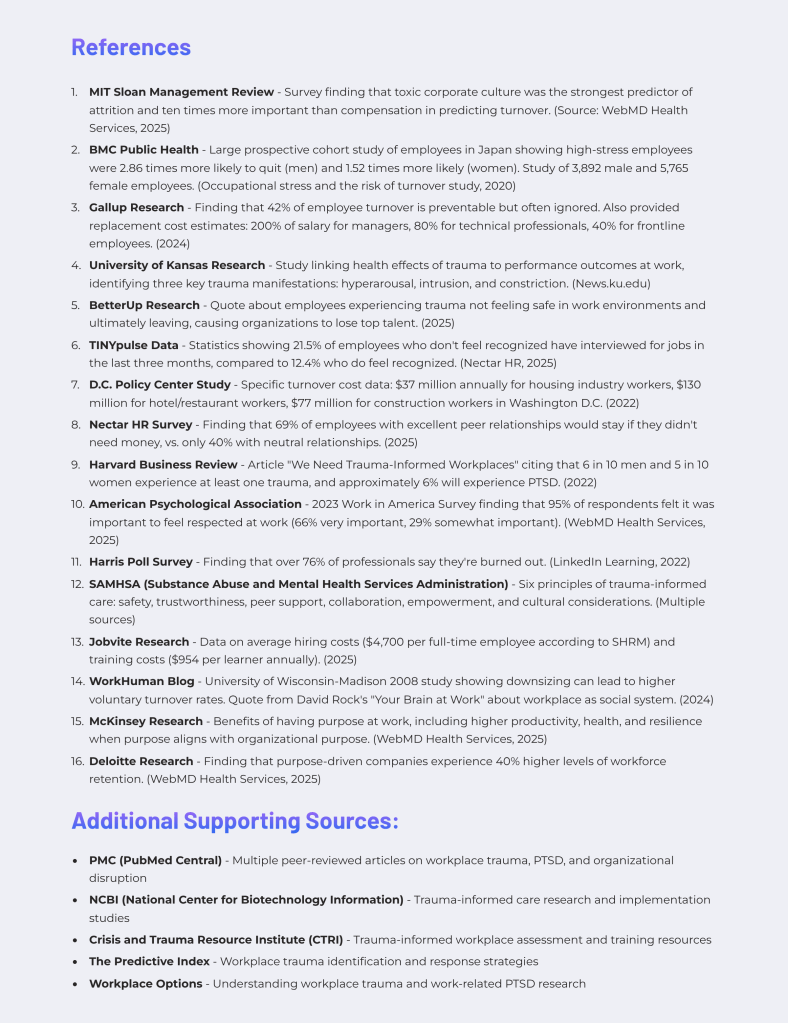
Here’s a list of trauma therapy techniques and models that are widely used to help individuals process and heal from traumatic memories:
Trauma Therapy Techniques and Models
- Eye Movement Desensitization and Reprocessing (EMDR):
- Uses guided eye movements or other forms of bilateral stimulation to help the brain process and integrate traumatic memories.
- Cognitive Behavioral Therapy (CBT):
- Focuses on identifying and changing negative thought patterns and behaviors associated with trauma. A specific form, Trauma-Focused CBT (TF-CBT), is often used with children and adolescents.
- Prolonged Exposure Therapy (PE):
- Involves gradual exposure to trauma-related memories, emotions, and situations to reduce the distress they cause over time.
- Somatic Experiencing (SE):
- Emphasizes the body’s role in trauma recovery, helping individuals release stored trauma through body awareness and physical sensations.
- Narrative Therapy:
- Encourages individuals to rewrite their trauma story, reframing their experiences and separating their identity from the traumatic event.
- Internal Family Systems (IFS):
- Helps individuals identify and heal different “parts” of themselves that may hold trauma, such as protective or wounded parts.
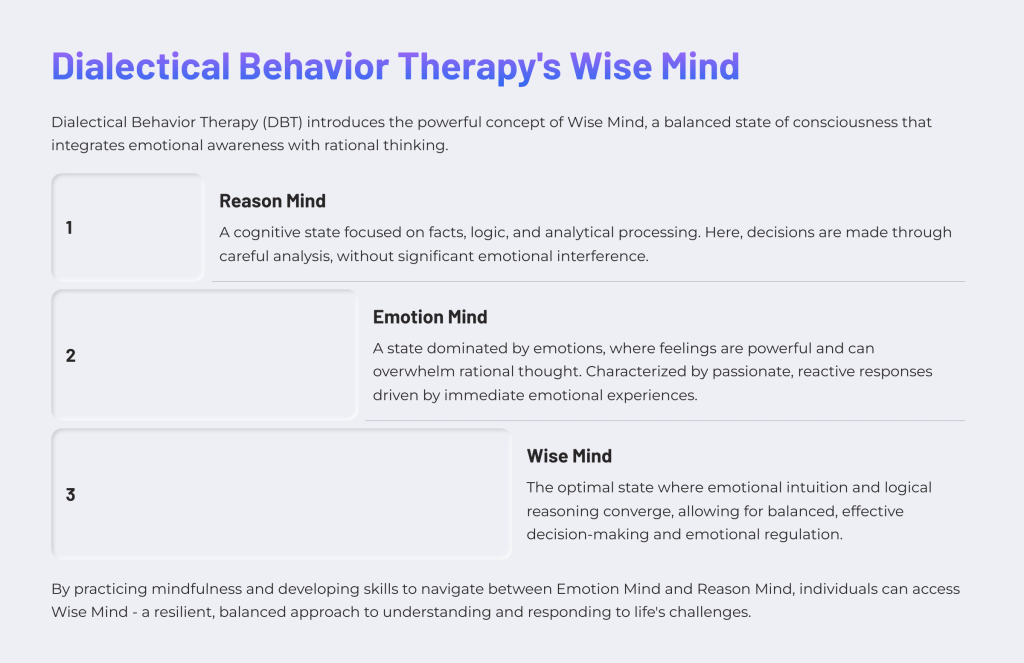
- Dialectical Behavior Therapy (DBT):
- Combines CBT techniques with mindfulness, distress tolerance, and emotion regulation, which are especially helpful for trauma survivors with complex emotional responses.
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT):
- A specialized form of CBT designed specifically for trauma, often involving both the individual and their caregivers.
- Psychodynamic Therapy:
- Explores unconscious patterns and past experiences that influence current behavior, often delving into childhood trauma.
- Brainspotting:
- Utilizes eye positioning to identify, process, and release trauma stored deep in the brain.
- Sensorimotor Psychotherapy:
- Integrates somatic (body-based) therapy with cognitive and emotional processing to address how trauma affects the body.
- Mindfulness-Based Stress Reduction (MBSR):
- Uses mindfulness and meditation techniques to increase awareness and acceptance of thoughts and feelings related to trauma.
- Accelerated Resolution Therapy (ART):
- Combines elements of EMDR with guided visualization to change the way traumatic memories are stored in the brain.
- Emotional Freedom Technique (EFT) / Tapping:
- Involves tapping on specific acupuncture points while focusing on traumatic memories, aiming to reduce emotional distress.
- Exposure and Response Prevention (ERP):
- Gradually exposes individuals to trauma-related triggers while helping them manage their responses, often used for PTSD and OCD.
- Hypnotherapy:
- Uses guided relaxation and focused attention to access and process trauma stored in the subconscious mind.
- Art Therapy:
- Encourages the expression of trauma through creative outlets like drawing, painting, or sculpture, facilitating emotional release and processing.
- Play Therapy (for children):
- Allows children to express and process trauma through play, a natural medium for young minds.
- Group Therapy for Trauma Survivors:
- Provides a supportive environment where individuals can share their experiences, learn from others, and gain a sense of community.
- Narrative Exposure Therapy (NET):
- Combines narrative techniques with trauma processing to create a coherent life story, particularly effective for survivors of complex trauma.
These techniques vary in their approaches but share the goal of helping individuals confront, process, and heal from traumatic memories. Each method can be tailored to the individual’s needs, allowing for a personalized path to recovery. Let me know if you’d like more information on these techniques!